Behaviour in dementia – an alternative view
Behaviours that challenge? Behavioural and Psychological Symptoms of Dementia (BPSD)? Dementia-related behaviour? Or is there sometimes a simpler way of looking at this?
Without dementia, our behaviour in response to our feelings is normally tempered by social norms and beliefs. However, in extreme circumstances, with no time or headspace for reflection or moderation, we act directly on our ‘fight or flight’ instincts. Lashing out at an attacker or trying to escape from extreme danger can be an appropriate response.
In most dementias, the person’s memory retains facts less and less reliably over time. But it continues storing the feelings generated by those facts. Therefore those feelings can exist without any factual context to explain them.
But we all need to make sense of our feelings before we can decide what to do about them. So we search for facts to fit those feelings. The recent facts are the most useful and normally the most accessible. But for people with dementia, that is often not the case. Feelings can easily get mis-matched to old or irrelevant facts.
Feeling fine without knowing why you feel that way is OK. But feeling even slightly ‘not OK’ with no explanation is not. Without context, those feelings can quickly escalate from uneasy to unnerving, and then to full-on distress. Unexplained distress can be deeply disturbing, even terrifying.
Trying to interpret feelings using out-of-date or misinterpreted facts can create a mismatch. This can result in seemingly odd or incongruous behaviour.
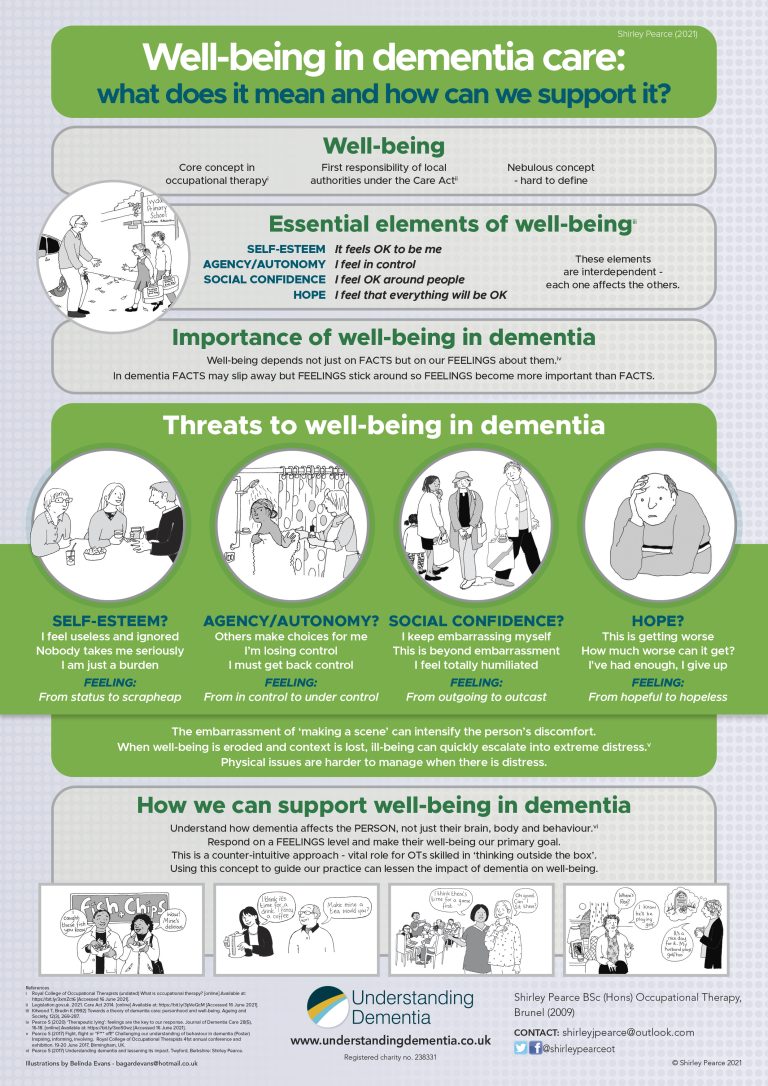
For carers, responding to behaviour we don’t understand can risk making the situation worse. So understanding the cause is key to making the person feel valued, free, accepted and safe. These are the four pillars of well-being.
Aggression – verbal or physical (unacceptable negative response) This can be a normal response to an abnormal situation – extreme fear, pain or frustration. In dementia the context may not be obvious, even to the person concerned. So quizzing them won’t help. They probably can’t get on to find our wavelength, so we need to try to find theirs. See also illusions, irrational behaviour and PTSD.
Dietary changes Dementia can affect the areas of the brain that process sensory information, including smell and taste. Even previously favourite foods can lose their appeal. However a liking for sweet things seems to increase over time, especially the comforting yumminess of chocolate. Moreover their memory may not have stored the facts of how long ago they last ate. They may not register the sensations of hunger or fullness. So it’s easy to see why people with dementia might accidentally miss a meal or eat twice.
Confabulation (fabricating experiences). Sometimes in everyday life we’re not sure what just happened. So we piece together the facts we have and then ‘join the dots’ to complete the picture. This is normal, and it requires some facts, then we combine memory, logic and common sense to fill the gaps.
Carer: The necklace isn’t in its place. Granny is forgetful and I remember her losing it before, so she’s ‘obviously’ misplaced it again.
Granny: The carer took it. Obviously. She must have done. That carer has daily access to my belongings.
However, neither of them saw what happened, so maybe they’re both wrong.
Mum: I noticed the clasp was damaged when the carer wasn’t there. I told Granny I’d get it mended.
But Granny’s memory didn’t store those facts.
The carer ‘jumped to the wrong conclusion’. But Granny ‘confabulated’, because that’s what people do when they have dementia. They both got it wrong for similar ‘joining the dots’ reasons, but we describe it very differently.
Crying for no apparent reason. We may not know why someone is crying. With limited access to recent facts, they might not know themselves. But upset feelings are real, so we shouldn’t dismiss them just because we don’t understand where they came from. Physical pain, frustration, sadness, unexplained loss or bewilderment may all be possible explanations.
Delusions aren’t behaviours – they’re false beliefs. In most types of dementia these are usually caused by illusions, misinterpretations or ‘joining the dots’ errors (see confabulation). However, some types of dementia (eg Lewy Body Dementia) can cause psychosis including delusions.
Disinhibited behaviour (behaving inappropriately in public). This can be because the context is missing (see paragraph 3). It may be acceptable at home but not in public. Alternatively it can indicate damage to brain areas governing impulse control, social and sexual behaviour, as in Fronto-Temporal Lobe Dementia.
Falls People with dementia are more likely to fall and there are many reasons (see illusions, incontinence, hoarding, sleep disturbances, pain, disinhibited behaviour, irrational behaviour, PTSD). Additionally, damage to the relevant part of the brain can affect balance and mobility.
Hiding (deliberately? really?) Someone may put something down somewhere that seems logical at the time, but they can’t find it later. That is easily done when our concentration lapses momentarily. See confabulation: the carer assumed Granny had ‘hidden’ her necklace. But she could have ‘misplaced’ it, if her daughter hadn’t taken it to be repaired.
Hoarding (keeping things ‘in case they come in useful’, even when that’s not likely). Some older people have lived through times of deprivation or shortages. This type of behaviour back then might have been normal, even sensible. But old habits can stick. When combined with memory changes in dementia, the result can be an apparently pointless accumulation of random things.
Illusions (misinterpretations by the brain when facts are missing). This can happen fleetingly to anyone when they are startled. Sensory impairment causes extra problems when combined with dementia. If we don’t see or hear clearly, we use memory to fill in the details (see confabulation). Could that loud bang just now have been a door slamming, or was it a firework or a dropped pan? It all depends on the context. See also PTSD. Has someone just gone out? Is it firework night? Is someone cooking or washing up? Or is this Edinburgh, with its daily One O’clock Gun?
Incontinence (escaped wee or poo). There can be a number of causes. Not getting there in time, not managing to hold on, leakage, not realising how urgently you need to go…. Factors include distraction, locating the toilet, managing clothing, mobility issues, constipation, infection, bowel disease etc. These can happen to anyone. But dementia can make them harder to manage, and ‘just in time’ can easily become ‘just too late’.
Irrational behaviour (behaviour with no obvious explanation). The person behaves in line with their feelings. But their feelings may relate to something the carer knows nothing about (see paragraph 4 re mismatch). See also illusions, PTSD.
Mood swings Recent factual memories give context to our feelings, so our mood often reflects recent events. But in advanced dementia, there are fewer reliable recent facts to go on. So someone’s feeling can easily trigger out-of-date and possibly traumatic memories, changing their mood instantly. (See also illusions, confabulation, PTSD.) Fortunately, it can improve just as quickly if we know how best to respond.
Paranoia (false belief of personal threat) – see illusions, hiding etc. The person’s memory may not store the facts of the item being moved. So ‘obviously’ someone hid it maliciously. However, unless we know the facts, we can’t assume that they didn’t either. Dementia makes people more vulnerable to financial and other abuse. So if they raise a concern, don’t dismiss it without checking. See also PTSD.
Perseveration (repeating an action or part of an action). The person’s memory may not have stored what they were in the middle of doing. So they can get ‘stuck’ part-way through the process.
Poor appetite Eating alone can be a cheerless activity; being watched as we eat can be distinctly off-putting. Eating is a multifaceted occupation and an important social ritual. Unless the person requires spoon-feeding, care workers often use the time to complete other tasks or paperwork. Care workers are rarely encouraged to eat with their clients, and may not even be allowed to do so. It’s best to make meals a social activity whenever possible. Give any help required as unobtrusively as possible to preserve their dignity. See also swallowing difficulties.
Post-traumatic stress disorder (PTSD) Some people with dementia have lived through horrific experiences. So their ‘joining the dots’ errors may trigger memories of past trauma. Such memories, without the right context to explain them, can become self-perpetuating. That must be unbearable.
Repetitive questioning (asking the same question over and over again). If the person’s memory hasn’t retained the answer, they won’t know what it is. So they may well ask again – and again. Sometimes the ‘correct’ factual answer doesn’t help. If the question indicates an underlying anxiety, we need to find an answer that will relieve it.
Restlessness (a feeling of wanting to get going and do something). The person’s memory may not store the facts – what they were about to do. So it can retain just that restless feeling. Alternatively there may be physical discomfort and/or lack of exercise (see also irrational behaviour, sundowning, wandering).
Seeing things differently This can be caused by damage to the back of the brain eg in posterior cortical atrophy (PCA). However, we normally rely on context to make sense of what our eyes see. So it can be simply be a misinterpretation or illusion,
Sleep disorders Disrupted routines, night staff in day clothes and noisy night-times can all make it hard to tell night from day. Daylight-type (blue toned) light in the evening and night can upset the body’s circadian rhythm (day/night). Inactivity and memory changes affect our ability to gauge the passage of time. Pain and anxiety can cause insomnia and some medications can cause sleep disturbance.
Social withdrawal (avoiding social situations one used to enjoy). Limited access to recent facts can lead to embarrassing social encounters. It can therefore become easier and less painful to stay away.
Sundowning (trying to leave a care facility in the afternoon/evening). Going home at the end of the day, or collecting children from school, may have been normal and habitual. Lack of recent facts can make someone’s surroundings feel unfamiliar, even if they have been living there for decades. So they may well feel as if they are out or away and less and less ‘at home’. So it is not very surprising if they want to leave (see also restlessness).
Swallowing difficulties These may be part of withdrawal or vegetation. Alternatively there may be a physical element as age and illness weakens throat muscles. The process of swallowing even occurs while we are asleep, but when we eat, it is under our conscious control. So in advanced dementia, knowing what to do next (see perseveration) in order to swallow can become a problem. Small quantities of soft, moist, appetising food go down more easily than anything hard or dry.
Vegetation (becoming passive and inactive). ‘Flop’ or ‘fawn’ behaviour can result when life becomes intolerable (see also PTSD), and the person appears to ‘give up’. This is related to the ‘freeze’ instinct, when frightened or injured animals instinctively keep still to avoid being spotted by predators. People with advanced dementia may refuse food and drink and becoming catatonic (immobile and unresponsive). We musn’t assume that they can’t hear us, or that they’ve lost their mind. Tender loving care is still important now (perhaps even more so), and a soothing voice may be comforting. Alternatively it can indicate hypoactive delirium. That is a medical emergency needing urgent intervention.
Wandering (walking somewhere, but being unable to find, or even identify, the intended destination). This can be linked to restlessness, lack of exercise or just a normal desire to go for a walk, combined with a memory that doesn’t store facts or places well. See also sundowning.
Withdrawal (becoming less responsive to others). This can happen when it all becomes too much and the person ‘gives up’ – see vegetation or it can indicate hypoactive delirium.
Many of these ‘behaviours that challenge’ might be better described as normal responses to challenging situations. So it’s often not the behaviour that’s the real problem. If there is underlying distress, that’s what we should be trying to ‘manage’. The first thing we need to do is validate the person’s feelings. Then tackle the cause and do our best to promote the person’s well-being.
Then we might see some of these behaviours begin to subside and they may even stop altogether. Or maybe we’ll just understand them differently…
See our main website to learn more about the Understanding Dementia approach.